Table of Contents
What Is EHR in Medical Billing?
Electronic Health Records (EHRs) in medical billing refer to how EHRs support and automate the financial side of healthcare. EHR systems manage patient data and link it directly to billing, insurance, and reimbursement processes.
What Does EHR Do in Revenue Cycle Management (RCM)?
EHR systems handle clinical data and convert it into billing-ready information. They:
- Track patient visits, diagnoses, and treatments
- Generate claims automatically using ICD-10 and CPT codes
- Connect with payers for eligibility checks and payment status
- Reduce billing delays by streamlining approvals and rejections
EHRs improve revenue cycle management by reducing manual errors and speeding up payments. This helps healthcare providers maintain a steady cash flow.
Always verify provider NPI numbers in your EHR. Missing/incorrect NPIs cause 23% of claim rejections (NPI Setup Guide).
EHR vs. EMR in Medical Billing: What’s the Difference?
| Feature | EHR | EMR |
|---|---|---|
| Data Sharing | Across practices & facilities | Internal use only |
| Billing Integration | Full RCM tools built-in | Limited billing features |
| Compliance | Supports HIPAA, MIPS, MACRA | Basic documentation only |
| Interoperability | Connects with labs, payers, EDI | Often standalone |
EHR is a complete system with financial, clinical, and administrative functions.
EMR focuses only on medical records for single providers and lacks billing automation.
How Does EHR Automate Medical Billing?
EHR automates billing tasks by:
- Auto-generating codes based on clinical notes
- Validating charges using payer rules
- Scrubbing claims before submission
- Capturing services and procedures in real-time
For example, the EHR can suggest matching billing codes when a doctor enters a diagnosis. This reduces coding mistakes and speeds up reimbursements.
🚀 Maximize Your Revenue – Get a Free Billing & Coding Assessment!”
“Discover hidden revenue leaks and boost reimbursements with our expert analysis.”
“Claim My Free Assessment →“
Why Traditional Billing Systems Fail
EHR is better than manual billing because it eliminates common issues like human errors, late payments, and compliance risks. Traditional billing systems rely on handwritten notes, disconnected tools, and manual data entry, increasing financial losses.
What Problems Do Manual Billing Systems Cause?
Manual billing creates avoidable issues:
- High error rates in coding and patient data
- Delayed reimbursements due to missing info or late submissions
- Non-compliance risks with HIPAA, MIPS, and MACRA rules
- Duplicate entries and billing mismatches
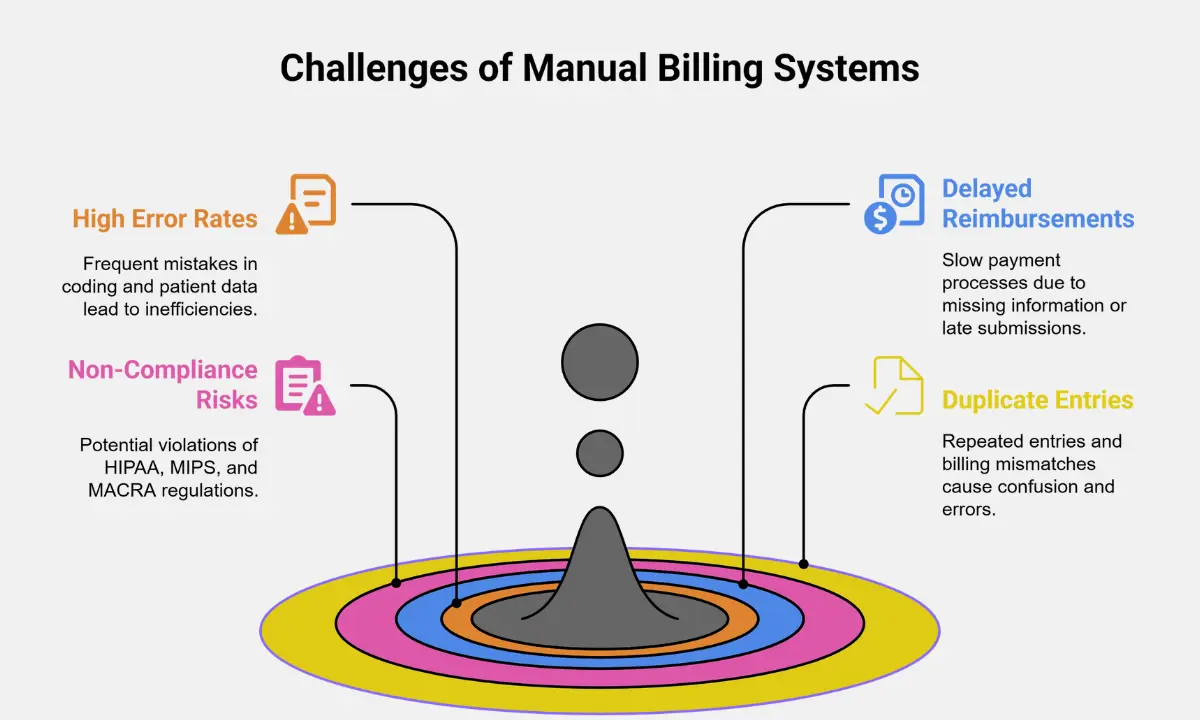
These problems reduce revenue and waste staff time. Clinics using paper-based billing often experience 15–30% more denials than digital systems.
Example: Claim Denials in Manual vs. EHR Billing
| System Type | Average Denial Rate | Common Causes |
|---|---|---|
| Manual Billing | 20%–30% | Coding errors, missing info |
| EHR-Based Billing | Under 10% | Auto-validation, rule checking |
EHR systems catch billing errors before submission. Manual systems often miss small mistakes that lead to full claim rejections.
Why ICD-10 and CPT Are Hard Without EHR
Manual billing struggles with ICD-10 and CPT coding because:
- Codes are complex and updated regularly
- Staff must search code books manually
- Mistakes in code selection lead to payment delays or audits
EHR tools solve this by auto-suggesting the correct codes from the diagnosis or procedure, using built-in logic and payer rules.
Manual billing processes are prone to errors and delays. For a step-by-step breakdown of how to modernize your workflow, see our guide: Medical Billing Process Workflow (Free PDF).
Benefits of EHR for Medical Billing
EHR billing advantages include faster medical claim processing, fewer denials, and higher coding accuracy. By automating key tasks, EHRs help clinics save time and increase revenue.
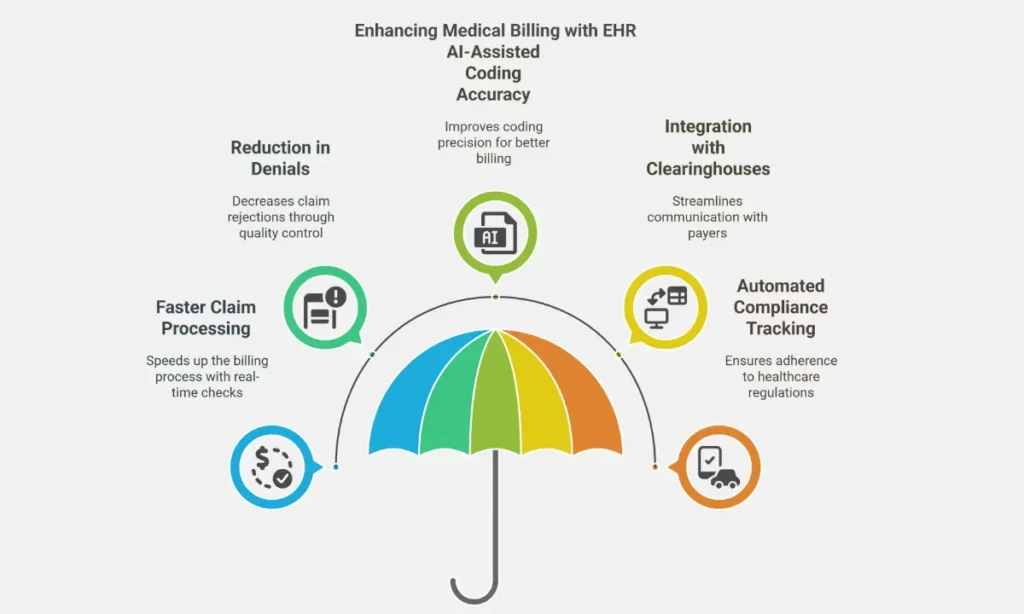
How Does EHR Speed Up Claim Processing?
EHR systems offer real-time eligibility checks. This means:
- Insurance status is verified instantly
- Patient coverage is confirmed before the service
- Claims are submitted faster with fewer rejections
Faster processing reduces payment delays and improves cash flow.
Learn More: Timely Filing Limit for Claims in Medical Billing
How Does EHR Reduce Denials?
EHRs use built-in claim scrubbing tools. These tools:
- Check claims for missing or incorrect data
- Flag coding mismatches before submission
- Apply payer-specific rules automatically
This reduces rejection rates by up to 60% compared to manual billing.
How Is Accurate Coding with EHR?
EHR systems use AI-assisted coding to improve ICD-10 and CPT accuracy. Features include:
- Code suggestions based on clinical notes
- Alerts for incompatible or outdated codes
- Automatic updates to coding databases
This improves billing accuracy and reduces audit risks.
How Does EHR Connect with Clearinghouses?
EHR systems integrate with clearinghouses and payer portals, enabling:
- Direct claim submission to insurers
- Real-time claim tracking
- Instant feedback on claim errors
This connection speeds up approvals and reduces back-and-forth communication.
How Does EHR Help with Compliance?
EHRs support automated compliance tracking for:
- HIPAA: Secure patient data handling
- MACRA & MIPS: Quality reporting and incentive tracking
- Audit preparation with proper documentation logs
Built-in compliance features reduce legal risks and support payer incentives.
What Is the Best EHR for Medical Billing in 2025?
The best EHR for medical billing in 2025 depends on the size and type of practice. Each EHR system offers specialized billing tools, pricing models, and interoperability strengths. Here’s a breakdown of the top options.
Which EHR Systems Offer the Most Efficient Billing Tools in 2025?
These five EHR systems are among the most used for billing in 2025:
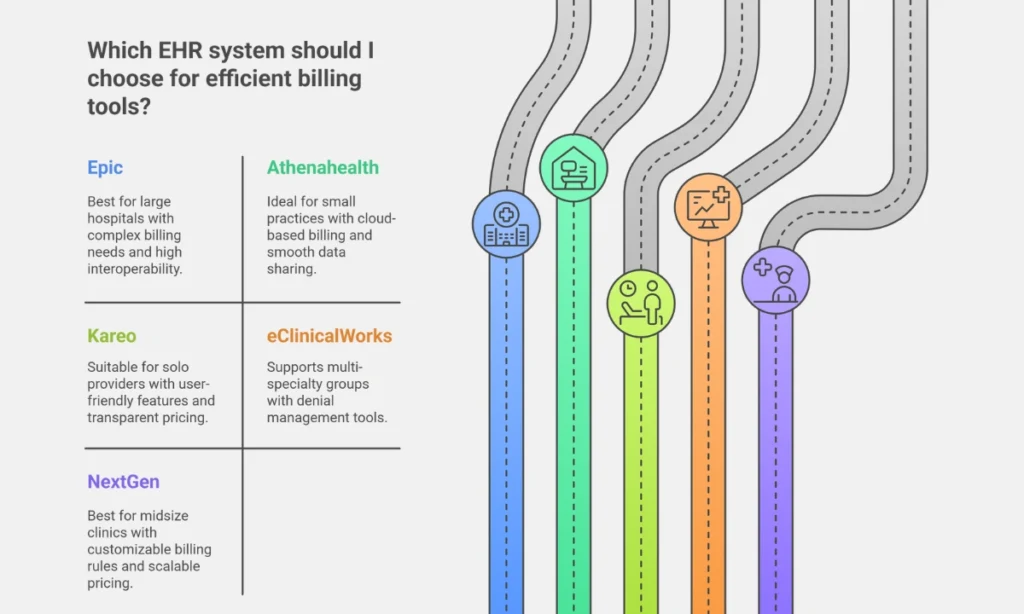
1. Epic
Epic suits large hospitals with complex billing needs. It includes advanced auto-coding and full revenue cycle management (RCM) tools. Epic offers custom pricing and supports high interoperability with other health systems.
2. Athenahealth
Athenahealth works well for small practices. It provides cloud-based billing with payer-specific rules. The pricing model is subscription-based, and interoperability is high, making data sharing smooth.
3. Kareo
Kareo (now part of Tebra) is a cloud-based practice management and billing solution for solo providers and small practices. Its features include a built-in coding assistant, real-time billing error alerts, and a transparent flat monthly fee. While its interoperability is moderate, Kareo remains a user-friendly choice for independent clinicians seeking streamlined revenue cycle management.
4. eClinicalWorks
eClinicalWorks supports multi-specialty groups. It includes a denial management tool and claims scrubbing features. It follows a tiered pricing model and provides strong interoperability.
5. NextGen
NextGen is suitable for midsize clinics. It allows for customizable billing rules and scalable pricing. It stands out for its strong interoperability features that support clinical and billing integrations.
Comparison Table: Best EHR for Medical Billing in 2025
| EHR System | Best For | Key Features | Pricing Model | Interoperability |
|---|---|---|---|---|
| Epic | Large hospitals | Auto-coding, RCM tools | Custom | High |
| Athenahealth | Small practices | Cloud billing, payer rules | Subscription | High |
| Kareo | Solo providers | Coding assistant, alerts | Flat monthly | Moderate |
| eClinicalWorks | Multi-specialty | Denial manager, claim scrubbing | Tiered | High |
| NextGen | Midsize clinics | Custom billing rules | Scalable pricing | Strong |
What Are the Most Common EHR Billing Problems in 2025?
EHR billing problems in 2025 mostly relate to system compatibility, coding errors, and workflow adoption. These issues can slow reimbursements, trigger claim denials, or cause compliance risks. Below are the key problems and proven solutions.
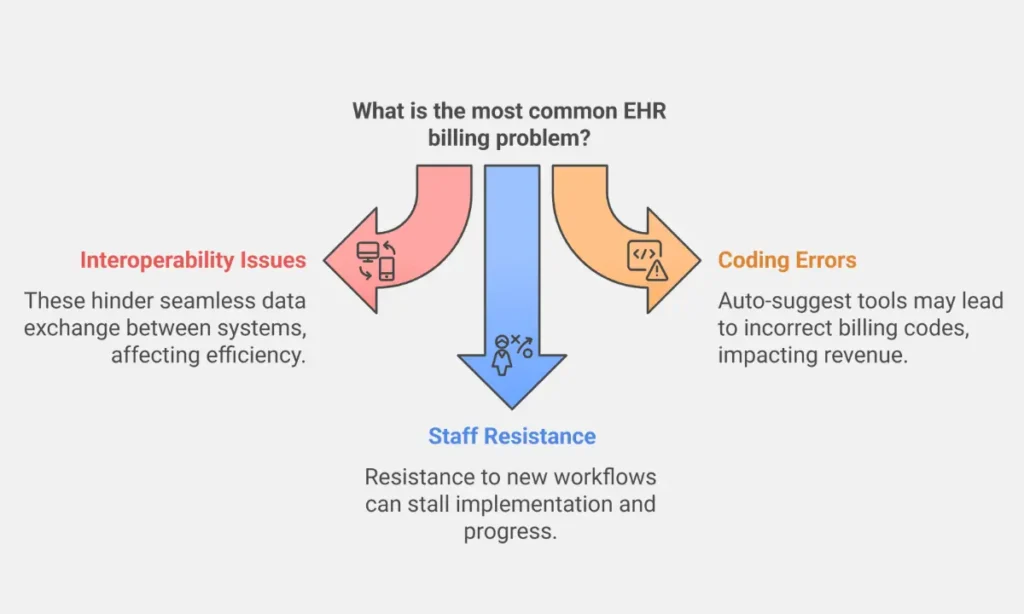
Which EHR Billing Problems Affect Practice Revenue the Most?
1. Interoperability Issues with Legacy Systems
Problem: Older systems often fail to sync with modern EHR platforms. This mismatch leads to data loss, claim delays, and manual re-entry.
Fix: Apply regular vendor updates and maintain patch compliance. These updates improve system compatibility and enable smoother data exchange across platforms.
2. Upcoding or Downcoding from Auto-Suggest Tools
Problem: Auto-suggested codes may lead to unintentional upcoding (billing too high) or downcoding (billing too low). Both cause audits or revenue loss.
Fix: Use AI-powered audit trails and coding validation tools. These features flag inconsistent entries and ensure billing aligns with clinical notes.
Many coding mistakes stem from confusing billing and coding roles. Clarify them with our guide: Medical Billing vs Coding.
3. Staff Resistance to New Billing Workflows
Problem: Team members may avoid adopting new billing features due to lack of training or unfamiliarity, reducing EHR efficiency.
Fix: Offer continuous staff training on EHR billing tools. Short, hands-on sessions improve confidence and billing accuracy.
Avoid audit risks, cross-check EHR data with our Compliance Checklist.
Overview: Problems and Fixes in EHR Billing
| Billing Problem | Impact | Solution |
|---|---|---|
| Interoperability with legacy systems | Data errors, delayed claims | Regular updates and patch management |
| Upcoding/downcoding from code suggest | Compliance risks, lost revenue | AI audits and coding validation |
| Staff resistance to new workflows | Low efficiency, error rates increase | Continuous billing feature training |
“Tired of Claim Denials? Let Our 97% Clean Claim Rate Work for You!“
“Outsource your billing, coding & credentialing services – and get paid faster, every time.“
“Claim My Free Assessment →“
Is EHR or EMR Better for Billing?
EHRs are better for billing than EMRs due to their broader functionality, billing interoperability, and integration with revenue cycle management (RCM) systems. EHR systems now serve as the standard for modern medical billing workflows.
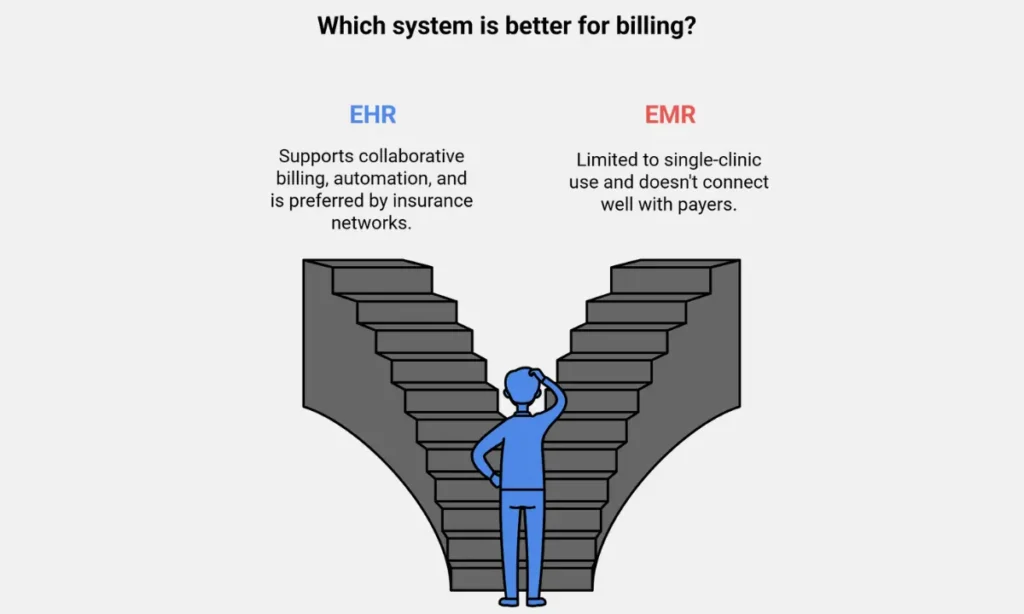
How Do EMR and EHR Differ in Billing Functions?
| System Type | Primary Use | Billing Capabilities | Interoperability |
|---|---|---|---|
| EMR | Internal patient records | Limited; lacks integration with payers | Low (single-provider only) |
| EHR | Multi-provider collaboration | Full RCM support, billing rule engines | High (cross-practice data) |
Why Is EHR the Standard for Medical Billing?
1. Supports End-to-End Revenue Cycle Management
EHRs handle eligibility checks, coding, charge capture, claim submission, and denial tracking in one platform.
2. Enables Cross-Practice Billing Integration
EHRs exchange billing data across systems, clearinghouses, and insurance networks, something EMRs can’t do.
3. Improves Claim Accuracy and Compliance
With features like real-time coding support and audit logs, EHRs reduce billing errors.
4. Complies with Industry Standards (e.g., HL7, FHIR)
EHR systems follow modern data exchange formats, ensuring billing interoperability.
What Are the Key EHR Billing Trends in 2025?
EHR billing trends in 2025 focus on automation, security, and efficiency. Technologies like AI, blockchain, and voice recognition are reshaping how healthcare providers manage claims, improve accuracy, and prevent denials.
How Is AI Changing EHR Billing in 2025?
AI in EHR billing predicts claim denial risks before submission. It analyzes coding patterns, payer behavior, and historical errors. This allows providers to fix issues early, improving claim approval rates.
- Forecast: By 2027, 40% of claim submissions will use AI-based prediction tools.
How Does Blockchain Improve Billing Security?
Blockchain in billing secures audit trails. Each transaction gets a time-stamped, tamper-proof record. This boosts transparency, helps meet compliance, and reduces billing fraud.
Used for:
- Claims auditing
- Identity verification
- Preventing double billing
How Is Voice Technology Used in EHR Billing?
Voice-to-text tools reduce manual entry by auto-filling billing fields based on spoken notes. Providers can directly dictate visit summaries, CPT codes, and billing details into the system.
Benefits:
- Faster documentation
- Fewer clerical errors
- Increased focus on patient care
Related Post:
How to Optimize EHR for Billing in 2025?
To optimize EHR for billing, clinics must focus on accuracy, staff readiness, system selection, and data-driven insights. These best practices improve cash flow, reduce denials, and enhance billing efficiency across all practice sizes.
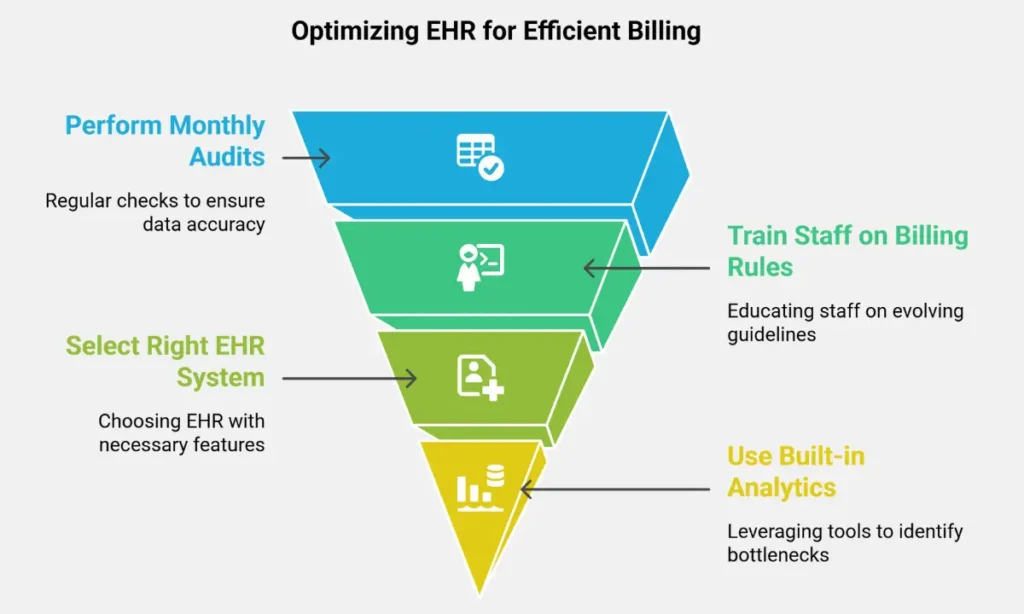
What Are the Most Effective EHR Billing Optimization Practices?
1. Perform Monthly Audits
Why: Regular audits help detect coding errors, missing data, or claim inconsistencies.
Impact: Prevents denials, boosts compliance, and improves documentation quality.
2. Train Staff on New Billing Rules
Why: Payer guidelines and EHR features evolve frequently.
How: Use short, focused sessions or vendor-led demos to update staff regularly.
3. Select the Right EHR System
What to look for:
Scalability: Can it grow with your practice?
Support: Is tech help responsive?
Payer Integration: Does it support clearinghouses, pre-authorization, and real-time eligibility checks?
4. Use Built-in Analytics
Function: Identify claim bottlenecks like slow payers, coding delays, or rejections.
Tool examples: Dashboards, RCM scorecards, claim aging reports.
Checklist: Ways to Optimize EHR for Billing
| Action | Purpose | Result |
|---|---|---|
| Monthly audits | Catch coding and billing errors | Reduced denials |
| Continuous staff training | Align with new rules and tools | Fewer mistakes, faster billing |
| Choosing scalable EHRs | Match system to practice growth | Long-term system efficiency |
| Using billing analytics | Monitor and fix claim issues | Faster collections, better forecasting |
FAQ’s on EHR Medical Billing
Can EHR reduce billing errors?
EHR systems reduce billing errors using automation, real-time validation, and coding support tools. These features flag mismatches and missing data before submission.
Which EHR is best for billing a small clinic?
Athenahealth and Kareo are best for small clinics. Athenahealth offers cloud billing with payer logic, while Kareo provides a coding assistant and fixed pricing.
How does EHR reduce claim denials?
EHRs reduce denials by applying payer rule engines, claim scrubbers, and AI-based validation. These tools detect errors before claims reach insurers.
Is EHR mandatory for billing in 2025?
No, EHRs will not be legally required for billing in 2025. However, they are highly recommended for faster reimbursement, compliance, and efficiency.
Recap: EHR improves billing accuracy, speed, and compliance
EHR systems improve billing by increasing accuracy, speeding up reimbursements, and ensuring compliance with payer rules. Whether running a solo clinic or a multi-specialty group, the right EHR makes billing smoother and more profitable.
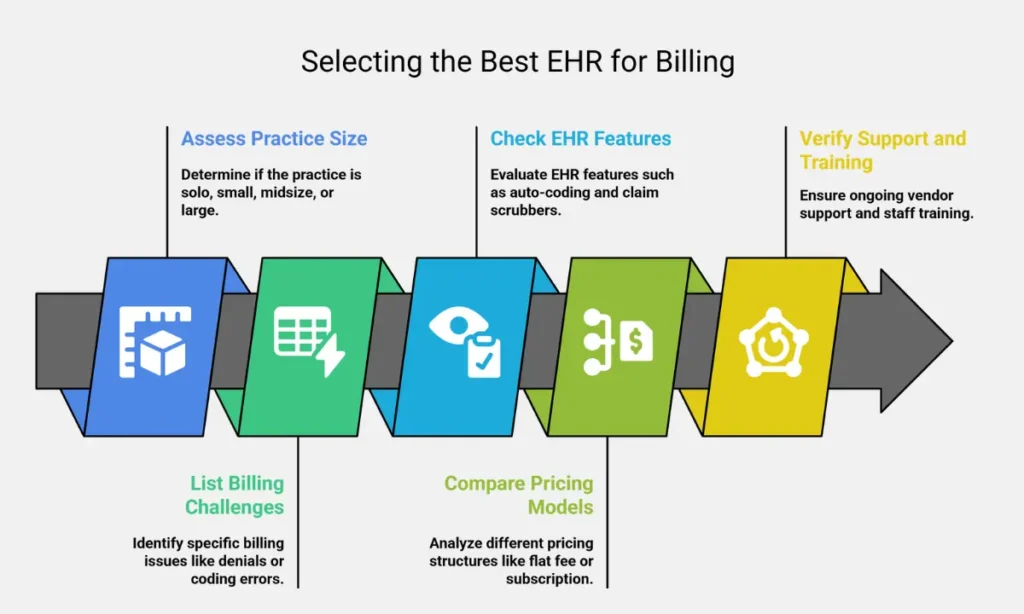
How to Choose the Best EHR for Your Billing Needs?
Use these steps to guide your EHR selection:
- Assess your practice size: Solo, small, midsize, or large.
- List billing challenges: Denials, coding errors, delays.
- Check EHR features: Auto-coding, claim scrubbers, and payer integration.
- Compare pricing models: Flat fee, subscription, scalable tiers.
- Verify support and training: Ensure ongoing vendor support and staff education.
“Billing + Coding + Credentialing – Fully Managed. Free Setup!“
“Get Started Now →“
Related Posts
- What is Medical Billing Outsourcing? Benefits, Challenges & How to Choose the Best Provider
- Rendering Provider vs Billing Provider: Key Differences, Compliance Strategies, and How to Prevent Costly Billing Errors
- Top 10 Best Medical Billing and Coding Companies in Texas
- Medical Coding Systems CPT, ICD-10, HCPCS