Medical billing compliance in 2025 demands more precision than ever. With evolving HIPAA rules, updated coding standards, payer-specific policies, and new CMS guidelines, every billing team must operate with structure and vigilance. Minor errors, like outdated code usage or missed documentation, can trigger costly denials, audits, or fraud investigations.
This checklist is built for billing managers, compliance officers, practice administrators, and healthcare providers. It breaks down the core areas your team must review regularly to align with federal, state, and payer requirements.
Use this as your annual reference guide across 10 key compliance domains.
Medical billing compliance in 2025 demands more precision than ever. Let MediBill RCM LLC handle the complexity—so you can focus on patient care.
🚀 97% Clean Claim Rate | 🚀 40% Faster Reimbursements | 🚀 Free Compliance Audit
Get Your Free Billing Assessment →“
Table of Contents
What are the 10 key areas of billing compliance in 2025?
Each area targets a core risk category identified by CMS, HHS, OIG, and private payers. The checklist helps mitigate legal exposure, maintain revenue integrity, and support ethical billing practices.
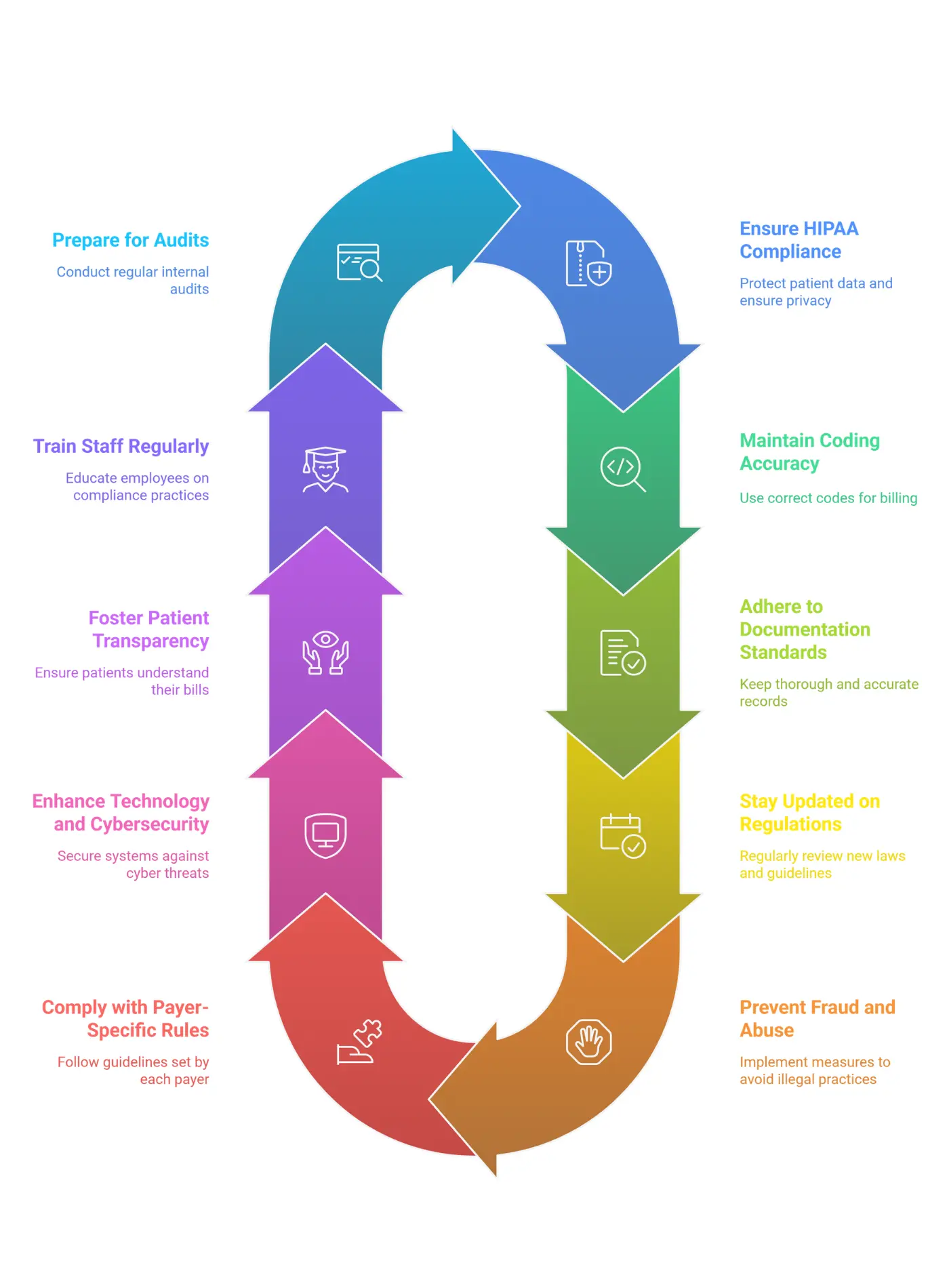
Why is HIPAA compliance critical for billing in 2025?
HIPAA violations remain a top enforcement priority for HHS and the Office for Civil Rights. With rising healthcare cyberattacks and increased reliance on digital billing systems, every billing department must reinforce its HIPAA security protocols, breach notification plans, and access controls.
What coding updates are required in 2025?
In 2025, CMS and the AMA will publish updated CPT and ICD-10-CM code sets. Practices must stop using outdated codes, ensure documentation supports medical necessity, and avoid coding errors like upcoding or unbundling. AI tools may assist, but human oversight remains essential.
How should documentation align with CMS guidelines in 2025?
Documentation must match CMS’s 2025 Evaluation & Management (E/M) guidelines and support every billed service in real-time. Signatures, dates, audit trails, and structured EHR inputs are necessary to defend claims in case of audits or payer disputes.
Read More: Medical Coding Systems CPT, ICD-10, HCPCS
What regulatory shifts will impact billing in 2025?
Key regulatory changes in 2025 include:
- The Medicare Physician Fee Schedule (MPFS)
- New rules under the No Surprises Act
- Updated Medicaid billing protocols by state
- CMS’s Final 2025 Telehealth Billing Guidelines
Billing teams must stay informed to avoid incorrect reimbursements and denials.
How can billing teams prevent fraud and abuse?
Fraud prevention requires proactive risk screening. In 2025, billing teams should regularly check the OIG Exclusion List, audit for red flags like duplicate billing, and enforce anonymous reporting systems. Medicare Advantage RADV audits continue to be mandatory for select organizations.
Avoid costly audits and denials with MediBill RCM’s end-to-end billing and compliance solutions. We manage:
- Coding Accuracy (CPT, ICD-10, HCPCS updates)
- HIPAA-Secure Billing (Encrypted claims, OIG monitoring)
- Payer Credentialing & Enrollment
📅 Limited 2025 Compliance Slots Available—Schedule a Consultation Today!
*Secure Your Practice Now →“
What payer-specific tasks should be tracked in 2025?
Each payer has unique requirements. Practices must:
- Track PTAN revalidations (every 3–5 years)
- Update fee schedules with commercial payers
- Monitor prior authorization rules for high-cost services
- Resolve denied claims within 30 days and analyze denial trends
Learn More: Timely Filing Limit for Claims in Medical Billing
What cybersecurity measures are required for billing software?
Cybersecurity compliance in 2025 focuses on:
- Aligning EHR systems with ONC 2025 Certification Criteria
- Conducting penetration testing annually
- Backing up billing data daily to HIPAA-compliant cloud systems
- Training staff quarterly on phishing and scam awareness
Read More: Top 10 EHR and Billing Software in the USA
How can practices improve patient billing transparency?
The No Surprises Act has increased patient rights around cost clarity. In 2025, practices must:
- Provide plain-language, itemized bills
- Offer pre-service cost estimates for non-emergency care
- Publicly display financial assistance policies
- Resolve billing complaints within 15 business days
What training is mandatory for billing and coding teams?
Compliance in 2025 requires:
- Annual training for billing/coding staff
- Updated coding education for providers
- Certification maintenance through AAPC or AHIMA
- Documented proof of training via logs or sign-in sheets
How should teams prepare for internal and external audits?
Audit preparedness reduces penalties and protects revenue. Practices should:
- Perform quarterly internal audits focused on risk areas
- Prepare for CMS Targeted Probe & Educate (TPE) audits
- Retain records for 7–10 years
- Develop Corrective Action Plans (CAPs) after audit findings
“Need more than a checklist? MediBill RCM’s certified team handles:
✅ Full-Service Medical Billing (Reduce denials by 60%)
✅ Provider Credentialing (Fast-track approvals)
✅ OIG Compliance Audits (Avoid penalties)
🔍 Get a FREE 2025 Compliance Gap Analysis (No obligation, 30-minute call)
*Claim Your Free Audit →“
Download the Full Medical Billing Compliance Checklist for 2025 PDF
Do you need a printable or shareable version? We’ve created a full PDF checklist with action items and space for internal notes. You can use it for team training, audit readiness, or compliance planning.
Related Posts
- Medical Billing Process: The Comprehensive 11-Step Workflow Guide (+Free PDF)
- Medical Billing vs. Medical Coding: Key Differences and Their Critical Roles in Healthcare
- How to Choose the Right Medical Billing Company for Your Practice in 2025?
- What is PC Ratio in Medical Billing? Definition, Calculation & Optimization
- Medical Claims Processing: A Comprehensive Guide to Processing, Challenges, and Innovations
- What is Medical Billing Outsourcing? Benefits, Challenges & How to Choose the Best Provider
- National Provider Identifier (NPI): What It Is and Why It Matters
- Rendering Provider vs Billing Provider: Key Differences, Compliance Strategies